Chapel Hill, NC
Cleveland, OH
Austin, TX
Washington D.C. area
Scottsdale, AZ
Seattle, WA
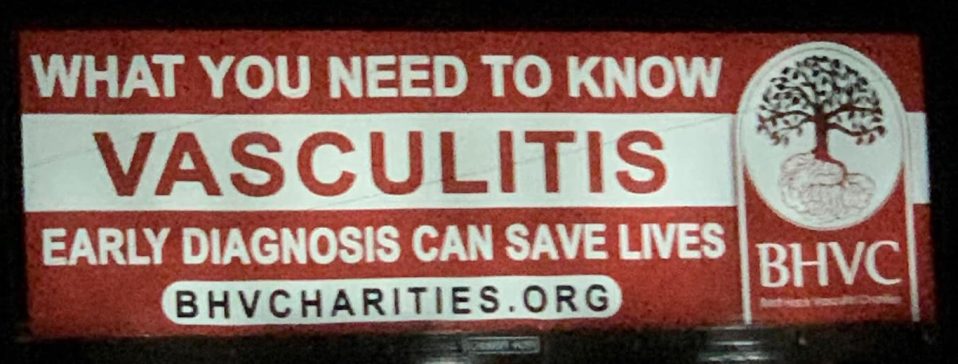
We are you. We are patients with vasculitis, care partners, friends, family, physicians, and researchers advocating for early diagnosis, better treatments, and improving quality of life for people with vasculitis.
Explore. Learn. Download Resources. Join a Support Group.
Pediatric Vasculitis
About Behçet’s Disease
Last Updated on February 5, 2024
Behçet’s disease or Behçet’s syndrome is a chronic and rare inflammatory condition. It involves inflammation of blood vessels (vasculitis) of different sizes (small, medium and large). It is unique compared to other vasculitic diseases in that it may involve blood vessels on both sides of the circulation (arterial and venous). The body tissues most frequently affected are the mucous-producing linings (mucosa) of mouth, eyes, gut, genitals as well as joints, skin, and nerves.
Behçet’s disease or Behçet’s syndrome is a chronic and rare inflammatory condition. It involves inflammation of blood vessels (vasculitis) of different sizes (small, medium and large). It is unique compared to other vasculitic diseases in that it may involve blood vessels on both sides of the circulation (arterial and venous). The body tissues most frequently affected are the mucous-producing linings (mucosa) of mouth, eyes, gut, genitals as well as joints, skin, and nerves.
There are studies that show that individuals with a certain genetic marker (HLA-B51) are more at risk of developing Behçet’s disease. However, many people without this gene can develop this disease. Some studies suggest that alteration of a person’s immune response or certain infections agents may play a role in the etiology of this disease. The cause of Behçet’s disease is remains unclear, and may likely be due to several factors coming together, including genetic risk factors, altered immune responses and an environmental trigger.
Although some of the symptoms of Behçet’s disease can resemble infections, it is important for patients and families to know that Behçet’s disease is not contagious or sexually transmitted, and it cannot be prevented.
Anyone can get Behçet’s disease. It is equally common in males and females. It develops in adulthood more often than childhood, though people of any age can develop symptoms and be diagnosed with Behçet’s disease. It is most common in people from Mediterranean countries (especially Turkey, 1 out of every 250 individuals), the Middle East (such as Israel, Iraq, and Iran), and Asia (especially China and Japan). These countries are along the historic “silk road”. However, people from any country and of any ethnicity can develop Behçet’s disease.
The symptoms of Behçet’s disease vary from person to person and range from mild to severe, depending on which parts of the body are affected. Two people with Behçet’s disease will likely have different “patterns” of symptoms.
Common symptoms of Behçet’s disease include:
- Recurrent episodes of painful sores or ulcers inside the mouth
- Painful sores or ulcers of the genitals
- Eye pain and inflammation
- Sores or bumps on the skin
Other symptoms of Behçet’s disease may include:
- Headaches
- Stomach pain
- Diarrhea
- Fevers
- Weight loss
- Fatigue
- Weakness
- Vision changes
- Leg swelling
- Difficulty breathing
- Chest pain
- Joint pain and/or swelling
Since Behçet’s disease is rare, many patients with possible Behçet’s disease will need initial investigations to rule out more common causes of their symptoms, such as infection or other autoimmune or inflammatory conditions. Behçet’s disease is a clinical diagnosis, meaning the diagnosis is made on the basis of a combination of symptoms, clinical features and results of tests. There is no specific, single diagnostic test for Behçet’s disease.
- Blood tests: Patients with Behçet’s disease may have some abnormal blood tests showing increased levels of inflammation (C-reactive protein, erythrocyte sedimentation rate).
- Eye examination: An eye exam performed by an ophthalmologist (eye doctor) may show inflammation in the front and/or back of the eye (uveitis) or inflammation of the blood vessels that supply the retina (retinal vasculitis).
- Tissue Biopsies: Sometimes, patients with possible Behçet’s disease may have a surgical procedure performed to remove a small sample of tissue (called a biopsy) from an affected vessel, skin or organ so that it can be looked at under a microscopy to help with the diagnosis
- Pathergy Test: Some patients may have a pathergy test performed in which a needle is used to prick the skin. If a papule or pustule forms at the site of the needle prick within 1 to 2 days, the person is considered to have a positive test. This is a possible sign of Behçet’s disease. However, this result should only be used in combination with other features because some individuals may have a positive pathergy test result without having Behçet’s disease while others with Behçet’s disease may have a negative result.
There are a variety of different medications that can be used to treat Behçet’s disease. Many of these medications are prescribed to decrease inflammation or dampen the immune system. These are called immune suppressants, and include corticosteroids, azathioprine, mycophenolate mofetil, cyclophosphamide, and/or biologic medications. Colchicine is frequently used as an anti-inflammatory medication for the treatment of oral and genital ulcers. Thalidomide or apremilast (a small molecule therapeutic) may be used for severe painful ulcers that are resistant to other treatments. Other drugs may be used to reduce the pain of ulcers or nerve involvement. There are also topical creams/ointments that may be prescribed to help reduce the pain or inflammation of the skin/mouth/genital sores.
The side effects will vary by medication, but can include nausea, vomiting, diarrhea, and a weakened immune system leading to increased risk for infections. Glucocorticoids (steroids) cause immunosuppression and possible other side-effects, including bone weakness (osteoporosis), elevated blood pressure, elevated blood sugar, trouble sleeping, increased appetite, and irritability. Particularly troublesome in children and youth is altered body image that can occur because of delayed growth, delayed puberty, weight gain, “round-face”, hairiness and stretch marks associated with prolonged prednisone treatment. Colchicine can cause stomach upset; most commonly it causes soft stools that are “manageable”. For the less frequently prescribed medications, it is important that patients and families talk to the prescribing doctor and pharmacist about possible side effects, as well as anything that you can do to protect against or test for some of these side effects. Your doctor might recommend that you have certain vaccinations to decrease risk of infection or blood/imaging tests if you are taking some of these medications.
Some patients with Behçet’s disease will have periods of time without any symptoms (called remission or inactive disease), followed by symptoms returning (often called a relapse, recurrence, or flare). Some medications can be prescribed during a flare to help reduce symptoms. If a patient is experiencing frequent flares or continued symptoms, their medication regimen might be changed to try to get better control of the inflammation.
Complications of Behçet’s disease, especially if untreated or uncontrolled, include vision changes which can progress to blindness, blood clots which can cause leg swelling or difficulty breathing, weakness/neurologic changes like stroke, or weakening of blood vessels (called aneurysms) which can burst and cause internal bleeding and even death.
The symptoms of Behçet’s disease and diagnostic criteria are the same in adults and children, especially after puberty, but it may take longer for children to get diagnosed with Behçet’s disease since it is quite rare. Also, the effects of the disease or treatments during fundamental periods of physical growth and psychological development will differ in children versus adults.
Patients with Behçet’s disease may need to see a variety of different subspecialists for monitoring and management of their symptoms. These typically include a rheumatologist, ophthalmologist (eye doctor), and dermatologist (skin doctor). Depending on the specific symptoms, other specialists may be involved such as neurologist (brain and nervous system doctor), gastroenterologist (GI doctor), gynecologist or urologist (specialists in female and male reproductive systems), pulmonologist (lung doctor), and cardiologist (heart doctor).
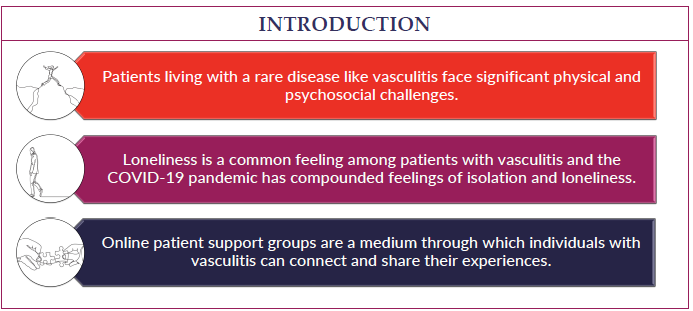
Behçet’s disease can be distressing to patients and their family members, especially if patients are experiencing significant discomfort or symptoms. It is important for patients to have a strong support system of family and friends, and to get plenty of rest, exercise, and healthy food intake for their overall health.
There is no cure for Behçet’s disease, but there are treatments that can reduce symptoms of pain, and inflammation. There are some dangerous complications of Behçet’s disease that have the potential to cause serious problems, so it is very important to see your doctor regularly and follow their treatment recommendations to keep the disease controlled, as well as contact them if any new symptoms start.
American Behçet’s Disease Association: https://www.behcets.com/
John Hopkins Vasculitis Center: https://www.hopkinsvasculitis.org/types-vasculitis/behcets-disease/
Behçet’s Disease Videos
Patient Perspective: Living with Behcet's Disease