Upcoming Venues:
Austin, TX
Washington D.C. area
Scottsdale, AZ
Seattle, WA
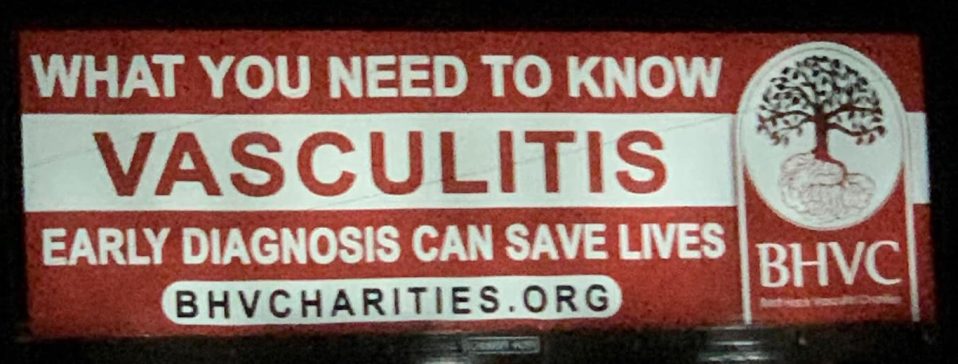
We are you. We are patients with vasculitis, care partners, friends, family, physicians, and researchers advocating for early diagnosis, better treatments, and improving quality of life for people with vasculitis.
Explore. Learn. Download Resources. Join a Support Group.
Vasculitis Types
About IgA Vasculitis
Last Updated on February 5, 2024
IgA (immunoglobulin A) vasculitis, formerly known as Henoch-Schönlein purpura, is a form of vasculitis—a family of rare disorders characterized by inflammation of the blood vessels, which can restrict blood flow and damage vital organs and tissues. IgA vasculitis causes inflammation of the small blood vessels of the skin, joints, intestines, and kidneys. Rarely, it can affect the lungs and central nervous system. It is the most common form of vasculitis in children.

Quick Facts

Varies greatly geographically 60-550 cases per million worldwide

2 per 100,000 US cases

Any onset age, but 90% are children 3-10 years of age

More common in children. Adults tend to have more severe disease.

Equally split between males and females

More common in Caucasians or people of Asian descent
IgA (immunoglobulin A) vasculitis, formerly known as Henoch-Schönlein purpura, is a form of vasculitis—a family of rare disorders characterized by inflammation of the blood vessels, which can restrict blood flow and damage vital organs and tissues. IgA vasculitis causes inflammation of the small blood vessels of the skin, joints, intestines, and kidneys. Rarely, it can affect the lungs and central nervous system. It is the most common form of vasculitis in children.
IgA vasculitis is systemic, meaning it can affect multiple organ systems in the body. The most characteristic symptom is a purplish skin rash that resembles bruises, mostly affecting the legs and buttocks. Other common symptoms or signs of organ involvement include abdominal pain, joint pain and swelling, and kidney inflammation.
When IgA vasculitis occurs in children younger than 16 years old, it is usually self-limited because most patients recover on their own within one to two months without treatment. Adults may have more severe and relapsing disease requiring immunosuppressive treatment. If the kidneys and intestines are affected, medical treatment is often needed, and ongoing medical follow-up is necessary.
The exact cause of IgA vasculitis is not fully understood. Vasculitis is classified as an autoimmune disorder, a disease that occurs when the body’s natural defense system mistakenly attacks healthy tissue. In IgA vasculitis, the immunoglobulin A antibody—a type of antibody that works to fight infections—is thought to play a role in blood vessel inflammation.
Studies show that 75 percent of people with IgA vasculitis develop the disease after an upper respiratory or gastrointestinal (GI) infection. Other possible triggers for IgA vasculitis include certain medicines, food reactions, insect bites, some vaccinations and, rarely, cancer. Although IgA vasculitis is seen throughout the year, there is an increase in cases during the fall and winter months. It is not considered contagious.
IgA vasculitis can affect people of any age, but 90 percent of patients are children aged 3 to 10 years. It is more common in boys than in girls. Adults tend to have more severe disease than children, and therefore may be treated more aggressively.
In adults, the annual incidence of IgA vasculitis in the United States is approximately 2 cases per 100,000 adults.
Patients with IgA vasculitis may experience several weeks of headache, fever, and muscle aches before the primary symptoms set in:
- Rash: A raised, reddish-purple rash called purpura is the characteristic symptom that helps doctors diagnose the disease. Lesions develop primarily on the buttocks, legs and feet, but can also affect the elbows, arms, and trunk.
- Arthritis: Painful, swollen joints, especially affecting the knees and ankles. The arthritis generally goes away on its own without causing permanent joint damage.
- GI problems: Stomach pain, nausea, vomiting, or bloody stools, which can occur before, during or after the rash.
- Kidney inflammation: Blood or protein in the urine, detected in urinalysis test. Kidney inflammation usually dissipates as IgA vasculitis resolves, with most patients recovering completely. However, in some cases, IgA vasculitis can cause kidney damage/failure, and dialysis or a kidney transplant may be needed.
Rarely, IgA vasculitis can cause bowel bleeding or bowel obstruction—a severe complication caused by the bowel folding onto itself. Kidney failure is another potential complication, especially in adults.
There is no single test for diagnosing IgA vasculitis. Your doctor will consider several factors including a detailed medical history, physical examination, laboratory tests, and specialized imaging studies. A skin biopsy is frequently needed to help diagnose IgA vasculitis.
- Laboratory tests: Blood tests and urinalyses can help rule out other diseases and detect signs of infection, anemia or kidney disease.
- Imaging studies: These may include ultrasound (abdominal, scrotal/testicular, X-rays (chest, abdomen), magnetic resonance imaging (MRI) to assess for neurological complications, and/or computed tomography (CT) scans of the head or abdomen.
- Biopsy: This surgical procedure removes a small tissue sample from an affected organ, which is examined under a microscope for signs of inflammation or tissue damage. In IgA, a skin biopsy typically shows vasculitis with deposits of immunoglobulin A. A kidney biopsy is sometimes necessary.
Symptoms of IgA vasculitis typically last one to two months and most patients recover on their own without treatment. Therefore, treatment is usually aimed at relieving symptoms until they dissipate. The following medications may be prescribed:
- Antibiotics (if an infection is suspected to be causing the IgA vasculitis)
- Over-the-counter medications for pain such as acetaminophen
- Anti-inflammatories such as ibuprofen for joint pain and swelling
- Glucocorticoids such as prednisone for severe stomach pain or kidney disease (Glucocorticoids are prescribed cautiously due to potentially serious side effects and should be avoided in children.)
In cases where the kidneys are affected or damaged, patients may require other medications that suppress the immune system.
Some IgA patients may need to take immunosuppressive drugs including glucocorticoids. These medications can have potentially serious side effects such as lowering the body’s ability to fight infection, and potential bone loss (osteoporosis), among others. Therefore, it’s important to see your doctor for regular checkups. Medications may be prescribed to offset side effects. Infection prevention is also very important. Talk to your doctor about getting vaccines (e.g., flu shot, pneumonia and/or shingles vaccination), which can reduce your risk of infection.
About one-third of individuals who have IgA vasculitis will experience a relapse, typically several months after the initial episode. Symptoms are usually less severe during a relapse. If your initial symptoms return or you develop new ones, report them to your doctor as soon as possible. Regular doctor visits and ongoing monitoring of laboratory and imaging tests are important in detecting relapses early.
Effective treatment of IgA vasculitis may require the coordinated efforts and ongoing care of a team of medical providers and specialists. In addition to a primary care provider, IgA patients may need to see the following specialists:
- Dermatologist (skin)
- Gastroenterologist (digestive system)
- Rheumatologist (joints, muscles, immune system)
- Nephrologist (kidneys) or others as needed
The best way to manage your disease is to actively partner with your health care providers. Get to know the members of your health care team. It may be helpful to keep a health care journal to track medications, symptoms, test results and notes from doctor appointments in one place. To get the most out of your doctor visits, make a list of questions beforehand and bring along a supportive friend or family member to provide a second set of ears and take notes.
Remember, it’s up to you to be your own advocate. If you have concerns about your treatment plan, speak up. Your doctor may be able to adjust your dosage or offer different treatment options. It is always your right to seek a second opinion.
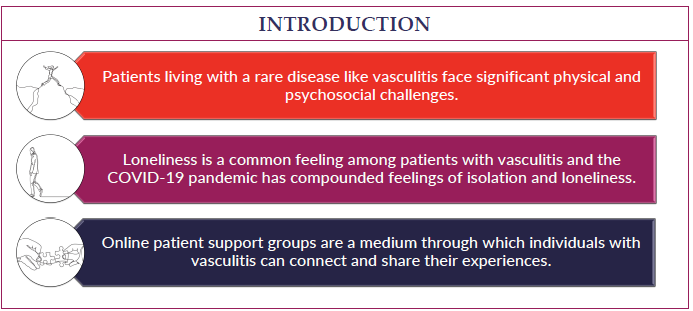
Although IgA vasculitis is not chronic for most patients, it can be, especially for adults. Living with a chronic condition can be overwhelming at times. Fatigue, pain, emotional stress, and medication side effects can take a toll on your sense of well-being, affecting relationships, work, and other aspects of your daily life. Sharing your experience with family and friends, connecting with others through a support group, or talking with a mental health professional can help.
There is no cure for IgA vasculitis at this time. In general, children with IgA vasculitis have an excellent prognosis. In adults, the disorder can be chronic. Most patients with this form of vasculitis fully recover within eight weeks and few have ongoing symptoms. Because relapses can occur, follow-up medical care is essential. Patients whose kidneys are affected need treatment and ongoing monitoring.
IgA Vasculitis Videos
Research Insights: Improving Diagnostics and Treatment of Small-Vessel Vasculitis
Vasculitis and the Skin Q&A