Chapel Hill, NC
Cleveland, OH
Austin, TX
Washington D.C. area
Scottsdale, AZ
Seattle, WA
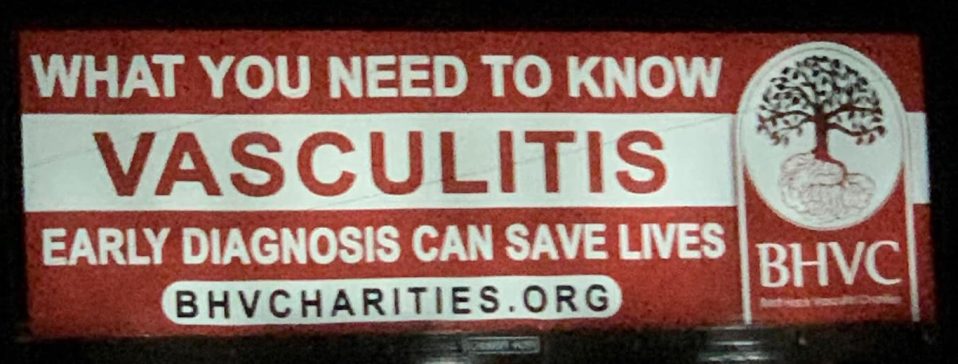
We are you. We are patients with vasculitis, care partners, friends, family, physicians, and researchers advocating for early diagnosis, better treatments, and improving quality of life for people with vasculitis.
Explore. Learn. Download Resources. Join a Support Group.
Pediatric Vasculitis
About Granulomatosis with Polyangiitis
Last Updated on February 5, 2024
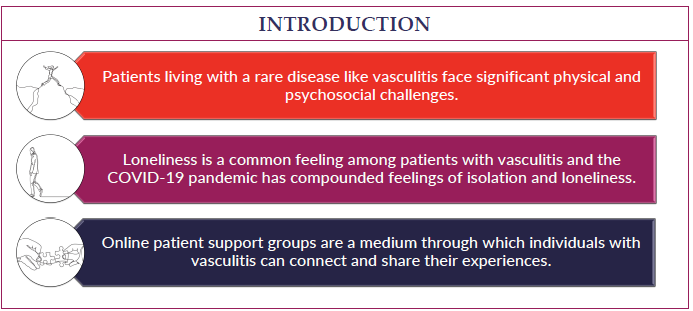
Granulomatosis with polyangiitis, formerly known as Wegener’s granulomatosis, is a rare autoimmune disease in which the body’s immune system mistakenly attacks its own body. It is a type of vasculitis, which means the immune system attacks the body’s blood vessels, causing inflammation. In GPA, small and medium sized blood vessels are affected. These involved vessels normally supply blood to organs all over the body, including kidneys, lungs, brain, skin, sinuses, and gastrointestinal tract. When inflammation is present, blood flow to these organs may be impaired resulting in dysfunction and damage.

Granulomatosis with polyangiitis, formerly known as Wegener’s granulomatosis, is a rare autoimmune disease in which the body’s immune system mistakenly attacks its own body. It is a type of vasculitis, which means the immune system attacks the body’s blood vessels, causing inflammation. In GPA, small and medium sized blood vessels are affected. These involved vessels normally supply blood to organs all over the body, including kidneys, lungs, brain, skin, sinuses, and gastrointestinal tract. When inflammation is present, blood flow to these organs may be impaired resulting in dysfunction and damage.
We do not currently know the cause of GPA. However, like many other autoimmune diseases, it is suspected that a combination of increased genetic risk and/or an unknown environmental trigger such as an infection, a pollutant, a medication, or allergen likely play a role. Researchers are still trying to find the cause. GPA is not preventable nor is it contagious.
GPA is a rare disease that can affect people of any age but mostly occurs in adults with an average age of 45 years. There are about 1-2 cases per 100,000 adults in the United States. It occurs in children much less frequently, estimated to be approximately one-tenth of the incidence in adults. Slightly more adult men get GPA than women, but in children, slightly more girls are affected than boys.
Since there are small and medium-sized blood vessels throughout the body, GPA can affect nearly any organ. Symptoms often vary from person to person. Most often the first symptoms are not specific and can include fever, loss of appetite, weight loss, skin rashes, and muscle/joint pain. As the disease progresses and organs are affected, more symptoms develop. The most common organs involved are the lungs, kidneys, skin, and sinuses.
Symptoms seen in GPA can include:
- Fever
- Fatigue
- Weight loss
- Joint pain or swelling
- Skin rashes
- Runny nose or nosebleeds
- Sinus congestion or pain
- Hearing problems
- Shortness of breath
- Cough, sometimes with blood
- Dark, frothy, or bloody urine
GPA can be a difficult disease to diagnose because it can present in so many different ways. Blood and urine tests are helpful in making the diagnosis, and often imaging studies or biopsies are required. Some patients may be diagnosed as an out-patient, but many are admitted to the hospital at the time of presentation because of severity of symptoms.
- Blood tests: Most people with GPA have antibodies present, called anti-neutrophil cytoplasmic antibodies (ANCA). You may also be found to have antibodies to either proteinase 3 (PR3) or myeloperoxidase (MPO), the former seen more often in GPA. A minority of patients with GPA will not have positive ANCA studies. Nonspecific lab findings include elevated markers of inflammation such as erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), platelets, and white blood count. Anemia is also common. Creatinine and BUN may be elevated in those with significant kidney involvement.
- Urine tests: Elevated levels of protein and/or blood in the urine suggest involvement of the kidneys.
- Imaging studies: x-rays (especially chest), echocardiogram, CT scans (lungs and sinuses), and MRIs may be necessary to evaluate for areas of inflammation and injury.
- Biopsies: These are often necessary to confirm a diagnosis of GPA or to assess how much the inflammation has affected an organ, such as the kidney. Most often, biopsies are performed on the kidney, sinuses, or lung.
- Pulmonary function tests (PFTs): These tests involve breathing in and out of a machine to evaluate how well your lungs function. If the PFTs are not normal, they may be monitored over time to assess the response to treatment.
Since GPA is caused by the immune system attacking the body, the overall objective of treatment is to quiet down the immune system and stop it from attacking the body. To do this, a group of medications called ‘immunosuppressants’ are used. Regardless of the medicine or combination of medicines that are used, the goal is to decrease the inflammation as quickly and as safely as possible to prevent damage to organs. The treatment program can be divided into two phases: remission-induction and remission-maintenance:
During the remission-induction phase, aggressive medications are started, which include glucocorticoids (prednisone or prednisolone by mouth, or methylprednisolone IV). Also, one of two other potent medications is usually given: cyclophosphamide or rituximab, if the disease is severe. The remission-induction phase lasts approximately 4-6 months, during which time the glucocorticoids dose is decreased and ideally discontinued. If the GPA is quiet at this time, the patient begins the remission-maintenance phase.
Medications commonly given to maintain remission of GPA include azathioprine, methotrexate or rituximab. It is not clear how long to continue medications during the maintenance phase. Most rheumatologists agree that at least two years of treatment is indicated to keep the GPA quiet. Many physicians will continue medications for longer, recognizing that flares (increase in disease activity) can occur in GPA. The hope is that the longer the GPA remains quiet, and in remission, the less chance it has of flaring.
In 2021 the American College of Rheumatology (ACR) published guidelines for the management of certain vasculitides, that were also endorsed by the Vasculitis Foundation (VF). Clinical practice guidelines are developed to reduce inappropriate care, minimize geographic variations in practice patterns, and enable effective use of health care resources. Guidelines and recommendations developed and/or endorsed by the ACR are intended to provide guidance for particular patterns of practice and not to dictate the care of a particular patient. The application of these guidelines should be made by the physician in light of each patient’s individual circumstances. Guidelines and recommendations are subject to periodic revision as warranted by the evolution of medical knowledge, technology, and practice.
Since most treatments for GPA suppress the immune system, they may affect the ability to fight infections. It is very important to make sure all appropriate vaccines, including for COVID-19, pneumonia and annual flu vaccinations are given either prior to or during treatment. (Note: live vaccines, such as MMR and chicken pox vaccination are avoided in people taking immunosuppressive medicines). Sometimes, an antibiotic, trimethoprim-sulfamethoxazole, is given during the remission-induction phase when there is more risk of infection due to immunosuppression. Glucocorticoids are known to cause a number of possible side effects in addition to immunosuppression which can include weight gain, acne, increased blood pressure, mood changes, difficulty sleeping, elevated blood sugar, and bone weakness. It may also interfere in the growth of growing children. As mentioned above, the goal is to try to wean entirely off or at least attain a very low dose of glucocorticoids by the end of the first 6 months of treatment.
Your medical team should discuss possible side-effects of all medications prior to starting treatment.
The goal of treatment is to remove the symptoms of GPA and quiet all the inflammation to prevent any damage to the body’s organs, while using the least amount of medicine necessary. If you do not respond fully to the first choice of medications, your doctor may switch to another medication to achieve remission. Once remission is achieved in GPA, the goal is to maintain this and avoid disease flares. If a flare does develop, it is important to be evaluated by your doctor and treated with medication as soon as possible in order to achieve remission again.
It is important to note that each person’s disease course is different. Some children may have a relatively mild course, with GPA affecting only sinuses, while others may be very sick at the time of diagnosis, having already sustained some injury to their organs, especially the kidneys and lungs. Complications from severe GPA can include kidney failure requiring dialysis, scarring of the lungs, injury to the sinuses, infections which could be related to the immunosuppressive medications, and very rarely, death.
Fortunately, much has been learned about diagnosing and treating GPA. More effective medications are being used more to treat GPA and the outcome for children with this diagnosis has improved significantly over the past few decades.
Overall, GPA is very similar in children compared to adults, but there are a few differences. As mentioned before, girls get more GPA when diagnosed in childhood, while in adults, GPA is more common in men. Childhood-onset disease also more often affects the nose, sinuses, and airway, whereas adult-onset disease more often affects the ears. Involvement in the rest of the body is similar between both adults and children. Most importantly, GPA may occur during very important times in physical, behavioral, and social development in children, and they may not be able to understand or cope with their disease as well as some adults can. It may be very helpful to receive mental health support to assist the you and the family at the time of diagnosis and during the course of treatment.
Since this disease can affect a number of different parts of the body, the medical treatment team tends to be large and include many specialties. In addition to the primary care doctor and the rheumatologist (autoimmune disease doctor), the team may include a pulmonologist (lung doctor), a nephrologist (kidney doctor), a gastroenterologist (stomach/intestines doctor), an otolaryngologist (ENT or ear, nose, and throat doctor), a neurologist (brain and nerves doctor), and a dermatologist (skin doctor). Additionally, many teams may include a counselor, psychologist and/or a psychiatrist to help out with the challenges of coping with a new diagnosis or hospitalization that may occur. Physical and/or occupational therapists may also be part of the team.
Having a chronic disease like GPA, no matter the severity, can be challenging to both the child and family. It is very important for the patient and family to receive the support they need through the medical team and other resources. Family and friend support is especially important at the time of diagnosis and subsequently. Talking with a mental health specialist, or connecting with other children with chronic diseases has been helpful to many. Having GPA as a child can have an impact on school attendance, academic performance, participation in school sports and other social activities. Receiving the necessary accommodations at school to maximize academic achievement is essential. (In the United States, families can obtain assistance in school via a 504 plan and/or an IEP as necessary). A social worker may be able to help navigate this process. It is also important to try to stay active physically and participate in hobbies and other activities which bring pleasure. Overall, having GPA does not mean that you cannot live the life you want to live. With appropriate treatment and regular follow up with the medical team, the main goal of treatment for everyone with GPA is to live a long and fulfilling life.
Information on current clinical trials is posted on the Internet at www.clinicaltrials.gov. All studies receiving U.S. government funding, and some supported by private industry, are posted on this government website. For information about clinical trials being conducted at the National Institutes of Health (NIH) in Bethesda, MD, contact the NIH Patient Recruitment Office:
Tollfree: (800) 411-1222
TTY: (866) 411-1010
Email: [email protected]
GPA Videos
Current Treatments for GPA and MPA including Avacopan
ACR_VF Guidelines: GPA-MPA Breakout
VF Patient Spotlight: Adisyn Wilson
Research Insights: Improving Diagnostics and Treatment of Small-Vessel Vasculitis
Research Insights: Targeting Antigen Specific B-Cells in ANCA associated vasculitis
TAVNEOS® (avacopan) ASN Perspectives_Geetha