Chapel Hill, NC
Cleveland, OH
Austin, TX
Washington D.C. area
Scottsdale, AZ
Seattle, WA
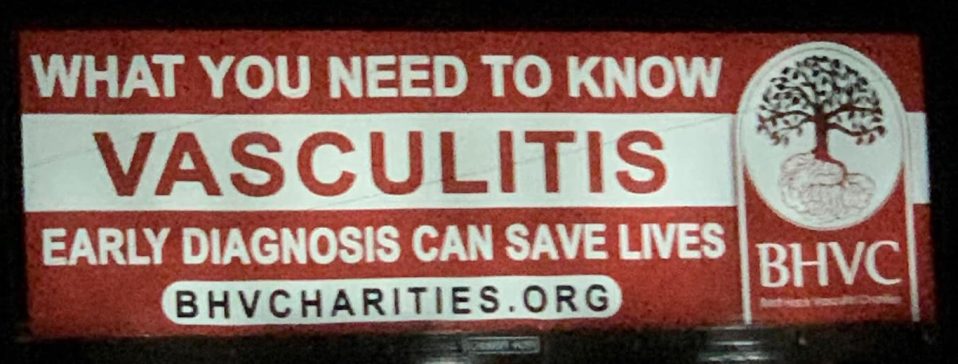
We are you. We are patients with vasculitis, care partners, friends, family, physicians, and researchers advocating for early diagnosis, better treatments, and improving quality of life for people with vasculitis.
Explore. Learn. Download Resources. Join a Support Group.
Vasculitis Types
About Polyarteritis Nodosa
Last Updated on February 5, 2024
Polyarteritis nodosa (PAN) is a form of vasculitis—a family of rare diseases characterized by inflammation of the blood vessels, which can restrict blood flow and damage vital organs and tissues. PAN affects medium-sized blood vessels, causing inflammation of the skin, nervous system, joints, kidneys, gastrointestinal (GI) tract, and heart, among other organs. Depending on the form of the disease, PAN may affect only the skin, a single body organ, or multiple organ systems.

Quick Facts

Number of cases worldwide unknown

3-4 per 100,000 US cases

Any onset age, but more likely between age 45-65

Rare in children

More common in males

Ethnic prevalence unknown
Polyarteritis nodosa (PAN) is a form of vasculitis—a family of rare diseases characterized by inflammation of the blood vessels, which can restrict blood flow and damage vital organs and tissues. PAN affects medium-sized blood vessels, causing inflammation of the skin, nervous system, joints, kidneys, gastrointestinal (GI) tract, and heart, among other organs. Depending on the form of the disease, PAN may affect only the skin, a single body organ, or multiple organ systems.
When PAN is systemic (affecting the whole body), symptoms can be wide-ranging, from fever, fatigue, weakness and weight loss to muscle and joint aches, skin lesions, numbness, and abdominal pain. High blood pressure is common due to kidney damage. Individuals with PAN are also at risk for an aneurysm—an abnormal bulge in a weakened artery wall that can rupture or bleed.
Prompt diagnosis and treatment are essential to prevent serious complications associated with PAN. The standard course of treatment includes glucocorticoids such as prednisone used in combination with other medications that also suppress the immune system. Even with effective treatment, PAN can be a chronic condition with periods of relapse and remission, so ongoing medical care is necessary.
The exact cause of PAN is not fully understood. Vasculitis is classified as an autoimmune disorder—a disease that occurs when the body’s natural defense system mistakenly attacks healthy tissue. The inflammatory process may be set in motion by a reaction to certain drugs or vaccines, or a bacterial or viral infection. PAN has been associated with hepatitis B infection. In most cases, however, the cause is unknown.
PAN is a rare disorder with an estimated annual incidence of 3 to 4 cases per 100,000 people in the United States. PAN can occur at any age; however, it is more likely to affect individuals who are between the ages of 45 to 65 years. The disease is more common in men than women.
Because PAN can affect so many organ systems, its symptoms may be wide-ranging. At onset, patients may experience fever, night sweats, weight loss, skin sores, and severe muscle and joint pains that develop over a period of weeks or months.
Other common symptoms include:
- Fatigue
- Loss of appetite
- Abdominal pain
- High blood pressure
- Blood in the stool
- Testicular pain in men
- Chest pain
- Difficulty breathing
- Numbness or tingling of the hands or feet
- Sudden loss of strength in the hands or feet
Potential complications can include aneurysms in the arteries of the kidneys, liver or GI tract, abdominal bleeding, blood clots in affected arteries, and tissue damage or loss in affected areas. The lungs are often spared.
There is no single test for diagnosing PAN. Your doctor will consider several factors including symptoms, a detailed medical history, physical examination, laboratory tests, and imaging studies. Your doctor will also attempt to rule out diseases with similar symptoms or characteristics. Laboratory tests can help support a diagnosis of PAN but are not conclusive on their own. A definitive diagnosis of PAN usually requires a specialized imaging study or tissue biopsy.
- Blood tests: Markers of inflammation (sedimentation rate and C-reactive protein) may be elevated.
- Imaging: If PAN is suspected, an angiogram—an X-ray taken during the injection of a contrast agent—may help confirm diagnosis. An angiogram can detect narrowing of the blood vessels or aneurysms. Computed tomography angiogram (CTA) or magnetic resonance angiogram (MRA) scans with dye may also be used to look for changes in blood vessels.
- Biopsy: A biopsy of affected tissue—surgical removal and analysis of a small tissue sample from an affected blood vessel or organ—is sometimes performed to confirm the diagnosis. For PAN, most biopsies are taken from skin, nerve or muscle tissue.
Treatment for PAN consists of glucocorticoids such as prednisone to reduce inflammation. In more severe cases, prednisone is combined with cyclophosphamide, a chemotherapy-type drug that blocks abnormal growth of certain cells, or other immunosuppressive drugs such as methotrexate, mycophenolate mofetil or azathioprine. High blood pressure needs to be well controlled. When PAN is related to hepatitis B, treatment often involves glucocorticoids, antiviral medications to treat the hepatitis, and sometimes plasma exchange.
In 2021 the American College of Rheumatology (ACR) published guidelines for the management of certain vasculitides, that were also endorsed by the Vasculitis Foundation (VF). Clinical practice guidelines are developed to reduce inappropriate care, minimize geographic variations in practice patterns, and enable effective use of health care resources. Guidelines and recommendations developed and/or endorsed by the ACR are intended to provide guidance for particular patterns of practice and not to dictate the care of a particular patient. The application of these guidelines should be made by the physician in light of each patient’s individual circumstances. Guidelines and recommendations are subject to periodic revision as warranted by the evolution of medical knowledge, technology, and practice.
The medications used to treat PAN have potentially serious side effects such as lowering your body’s ability to fight infection, and potential bone loss (osteoporosis), among others. Therefore, it’s important to see your doctor for regular checkups. Medications may be prescribed to offset side effects. Infection prevention is also very important. Talk to your doctor about getting vaccines (e.g., flu shot, pneumonia and/or shingles vaccination), which can reduce your risk of infection.
Even with effective treatment, relapses can occur in individuals with PAN. If initial symptoms return or new ones develop, report them to your doctor as soon as possible. Regular checkups and ongoing monitoring of lab and imaging tests are important in detecting relapses or new organ involvement.
Effective treatment of PAN may require the coordinated efforts and ongoing care of a team of medical providers and specialists. In addition to a primary care provider, patients with PAN may need to see the following specialists:
- Rheumatologist (joints, muscles, immune system)
- Cardiologist (heart)
- Gastroenterologist (digestive system)
- Nephrologist (kidneys)
- Dermatologist (skin)
- Neurologist (brain/nervous system); or others as needed
The best way to manage your disease is to actively partner with your health care providers. Get to know the members of your health care team. It may be helpful to keep a health care journal to track medications, symptoms, test results and notes from doctor appointments in one place. To get the most out of your doctor visits, make a list of questions beforehand and bring along a supportive friend or family member to provide a second set of ears and take notes.
Remember, it’s up to you to be your own advocate. If you have concerns about your treatment plan, speak up. Your doctor may be able to adjust your dosage or offer different treatment options. It is always your right to seek a second opinion.
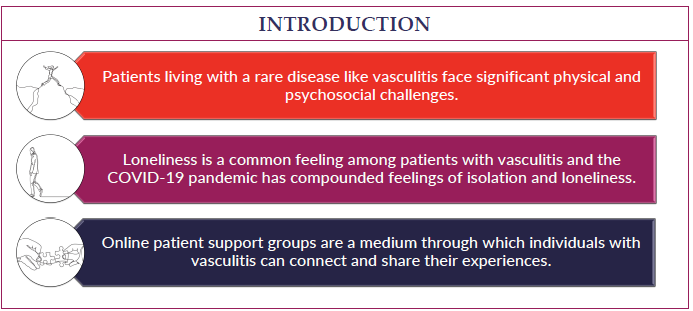
Living with a chronic condition such as PAN can be overwhelming at times. Fatigue, pain, emotional stress, and medication side effects can take a toll on your sense of well-being, affecting relationships, work, and other aspects of your daily life. Sharing your experience with family and friends, connecting with others through a support group, or talking with a mental health professional can help.
There is no cure at this time for PAN, but with prompt treatment and careful monitoring, many patients can achieve remission. The long-term prognosis depends on the severity of the organs involved. Because relapses can occur, follow-up medical care is essential.
Polyarteritis Nodosa Videos
ACRVF Guidelines Conf PAN Breakout