Chapel Hill, NC
Cleveland, OH
Austin, TX
Washington D.C. area
Scottsdale, AZ
Seattle, WA
We are you. We are patients with vasculitis, care partners, friends, family, physicians, and researchers advocating for early diagnosis, better treatments, and improving quality of life for people with vasculitis.
Explore. Learn. Download Resources. Join a Support Group.
Vasculitis Types
About Cutaneous Small-Vessel Vasculitis
Last Updated on February 5, 2024
Cutaneous small-vessel vasculitis (CSVV) is a form of vasculitis—a family of rare disorders characterized by inflammation of the blood vessels, which can restrict blood flow and damage vital organs and tissues. Formerly called hypersensitivity vasculitis, this disorder affects only the skin. CSVV was also previously known as angiitis, leukocytoclastic vasculitis, and allergic vasculitis.

Quick Facts

38-55 per million diagnosed

Unknown US cases

Any onset age, but usually over 16 years

IgA vasculitis more common in children

Slightly more common in males

More common in Caucasians
Cutaneous small-vessel vasculitis (CSVV) is a form of vasculitis—a family of rare disorders characterized by inflammation of the blood vessels, which can restrict blood flow and damage vital organs and tissues. Formerly called hypersensitivity vasculitis, this disorder affects only the skin. CSVV was also previously known as angiitis, leukocytoclastic vasculitis, and allergic vasculitis.
The typical symptoms of CSVV consist of a rash with tender, purple or reddish spots covering large areas—especially the legs, buttocks or torso—as well as hives, blisters, and open sores. CSVV can also be secondary to a systemic (affecting the whole body) vasculitis. In children, the disease can resemble IgA vasculitis (formerly called Henoch-Schönlein purpura), which also affects the small vessels of the skin and causes a similar rash.
CSVV is often triggered by a drug or by an infection, and usually clears up once the offending medication is discontinued, or the infection is treated. However, some patients will need glucocorticoids such as prednisone, sometimes used in combination with other medications, to control inflammation. Most cases go away within weeks to months. However, CSVV can be chronic, with periods of relapse and remission, so ongoing medical care may be necessary.
The exact cause of CSVV is not fully understood. Vasculitis is classified as an autoimmune disorder—a disease that occurs when the body’s natural defense system mistakenly attacks healthy tissue. CSVV can be caused by an allergic reaction to medications such as antibiotics, diuretics, and blood pressure medicines, as well as foods or food additives. Other triggers include upper respiratory tract or gastrointestinal infections and viruses such as hepatitis B or C, and HIV. Cancer is a rare but possible cause of CSVV.
CSVV can affect individuals with other autoimmune diseases such as rheumatoid arthritis, Crohn’s disease, systemic lupus erythematosus and Sjögren’s syndrome. CSVV can be part of certain forms of systemic vasculitis such as granulomatosis with polyangiitis, microscopic polyangiitis or eosinophilic granulomatosis with polyangiitis.
CSVV can occur at any age, but usually affects individuals over the age of 16. The disease occurs in females and males equally, although some studies indicate it is slightly more common in men. It most often affects Caucasians.
Approximately 38 to 55 per million adults per year are diagnosed with CSVV.
The hallmark symptom of cutaneous CSVV is a skin rash, with tender, purple or reddish-brown spots over the legs, buttocks and trunk, and sometimes the upper body. Other skin lesions include blisters, hives, and open sores (ulcers) with dead tissue. Crops of lesions typically appear over one or two days, with more appearing over the next days to weeks until treatment is initiated, or the allergy or other trigger goes away. Individual lesions can last up to three weeks and can leave scarring, especially if it ulcerates. CSVV is limited to the skin.
Skin lesions may result in non-healing ulcers and infections, thus good topical care of the skin is important.
There is no single test to diagnose CSVV. Your doctor will likely take a detailed drug history and ask about any current medications you’ve been taking, as well as recent infections. A typical evaluation includes a detailed medical history, a physical examination, blood and urine tests, and specialized imaging studies such as X-rays and computed tomography (CT) scans, when indicated.
A tissue biopsy is usually required to confirm diagnosis of CSVV. Biopsy is a surgical procedure that removes a small sample of affected tissue, which is examined under a microscope for signs of inflammation or damage. Usually, a biopsy of the skin rash showing inflammation of the small blood vessels confirms the diagnosis.
Treatment of CSVV starts with addressing the suspected underlying trigger. If a drug may have caused the disease, your doctor will probably advise you to discontinue it. If the medication is the culprit, your symptoms should disappear within a few weeks. Likewise, if an infection is the suspected cause, treating the infection may resolve symptoms. If the trigger was a food allergy, removing the offending food from the diet may help.
Because the legs are commonly affected by rash or joint pain, avoidance of prolonged standing may be helpful, along with elevation of the legs and use of compression stockings. To reduce inflammation in the blood vessels, your doctor may prescribe nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, naproxen or glucocorticoids.
In patients with more severe or ongoing skin rashes that are not due to infection, drugs such as colchicine, antihistamines, hydroxychloroquine, and dapsone (or a combination of these drugs) may be helpful to control symptoms.
In severe disease, a high-dose glucocorticoid may be required. In addition, other immunosuppressive drugs such as azathioprine, mycophenolate mofetil, or methotrexate may be prescribed.
Patients with disease in organs beyond the skin should be referred to a medical specialist for further evaluation.
The medications used to treat CSVV have potentially serious side effects such as lowering your body’s ability to fight infection, and potential bone loss (osteoporosis), among others. Therefore, it’s important to see your doctor for regular checkups. Medications may be prescribed to offset side effects. Infection prevention is also very important. Talk to your doctor about getting vaccines (e.g., flu shot, pneumonia and/or shingles vaccination), which can reduce your risk of infection.
Even with effective treatment, some individuals with CSVV will experience relapses. If your symptoms return or you develop new ones, report them to your doctor as soon as possible. Regular checkups and ongoing monitoring of lab and imaging tests are important in detecting relapses early.
Effective treatment of CSVV may require the coordinated efforts and ongoing care of a team of medical providers and specialists. In addition to a primary care provider, CSVV patients may need to see the following specialists:
- Rheumatologist (joints, muscles, immune system)
- Dermatologist (skin) or others as needed
The best way to manage your disease is to actively partner with your health care providers. Get to know the members of your health care team. It may be helpful to keep a health care journal to track medications, symptoms, test results and notes from doctor appointments in one place. To get the most out of your doctor visits, make a list of questions beforehand and bring along a supportive friend or family member to provide a second set of ears and take notes.
Remember, it’s up to you to be your own advocate. If you have concerns about your treatment plan, speak up. Your doctor may be able to adjust your dosage or offer different treatment options. It is always your right to seek a second opinion.
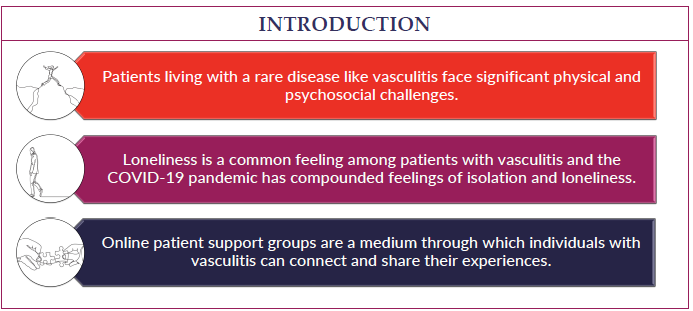
Living with a chronic condition such as CSVV can be overwhelming at times. Fatigue, pain, emotional stress, and medication side effects can take a toll on your sense of well-being, affecting relationships, work, and other aspects of your daily life. Sharing your experience with family and friends, connecting with others through a support group, or talking with a mental health professional can help.
There is no cure for all patients with CSVV, but most people have a good outlook, with the disease typically resolving within a few weeks or months. Some develop chronic, recurring disease, which can affect quality of life, and in those cases follow-up medical care is essential.
Cutaneous Small-Vessel Vasculitis Videos
Vasculitis and the Skin Q&A