Chapel Hill, NC
Cleveland, OH
Austin, TX
Washington D.C. area
Scottsdale, AZ
Seattle, WA
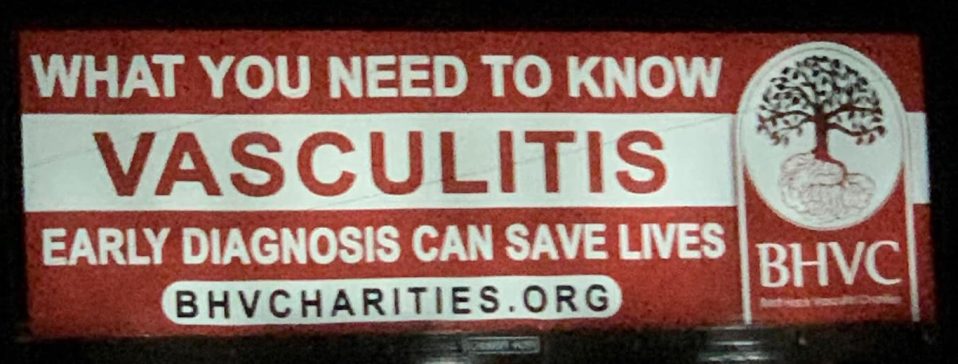
We are you. We are patients with vasculitis, care partners, friends, family, physicians, and researchers advocating for early diagnosis, better treatments, and improving quality of life for people with vasculitis.
Explore. Learn. Download Resources. Join a Support Group.
Vasculitis Types
About Behçet’s Syndrome
Last Updated on February 5, 2024
Behçet’s syndrome is a form of vasculitis—a family of rare disorders characterized by inflammation of the blood vessels, which can restrict blood flow and damage vital organs and tissues. Behçet’s affects blood vessels of all sizes and types, and can potentially involve any organ including the central nervous system. Treatment is essential in controlling symptoms and preventing serious complications such as blindness and stroke.

Quick Facts

Highest prevalence in Turkey; 400 per 100,000

3-5 cases per 100,000 in US

Most common in ages 20-30, but can occur at any age

Rare in children

Occurs in both males and females. May be more severe in males.

More common in people of Middle Eastern, Mediterranean, or Asian descent
Behçet’s syndrome is a form of vasculitis—a family of rare disorders characterized by inflammation of the blood vessels, which can restrict blood flow and damage vital organs and tissues. Behçet’s affects blood vessels of all sizes and types, and can potentially involve any organ including the central nervous system. Treatment is essential in controlling symptoms and preventing serious complications such as blindness and stroke.
Common symptoms of Behçet’s include painful mouth and genital sores, skin rashes, swollen joints, and eye inflammation. However, the disease also causes more serious symptoms such as vision loss, blood clots, gastrointestinal, brain and/or spinal cord problems.
Treatment depends on the severity of disease and organ system involvement. In mild cases, topical glucocorticoids may be applied to affected areas. For more serious disease, medications that suppress the immune system are used. Behçet’s is a chronic disease and relapses are common, thus ongoing medical care is important.
The cause of Behçet’s is not fully understood. Vasculitis is classified as an autoimmune disorder—a disease that occurs when the body’s natural defense system mistakenly attacks healthy tissue. Behçet’s is one of the few forms of vasculitis where a specific gene – HLA-B51 – is a known risk factor for the syndrome. However, this gene is also seen in the general population, and not everyone who has it gets Behçet’s. Therefore, it is believed that an infection and/or environmental factors may play a role in the onset of this disease.
Behçet’s mainly affects people in their 20s and 30s, but the syndrome can occur in individuals of all ages. While Behçet’s occurs in both men and women, the disease is usually more severe in males.
People from the Mediterranean, the Middle East and Asia are more likely to get this disease; it is rare in the US. Prevalence is estimated at 3 to 5 per 100,000 people in the US. Turkey has the highest prevalence, with approximately 400 cases per 100,000 people.
The symptoms of Behçet’s can vary greatly from person to person. Some may have milder disease, while others have severe, even potentially life-threatening symptoms. Most people have periods of relapse and remission, with symptoms often showing up in different parts of the body—sometimes years later.
The most common symptoms of Behçet’s syndrome are:
- Painful ulcers, resembling canker sores, inside the mouth
- Painful, open genital sores
- Skin lesions resembling acne that can occur anywhere on the body
- Eye inflammation with symptoms of blurred vision (or blindness), redness and pain
- Joint swelling, pain and stiffness, especially in the knees, ankles, elbows and wrists
Less common, but serious symptoms include:
- Blood clots
- Intestinal problems
- Inflammation of the brain and spinal cord, with severe headaches, stiff neck, and fever (meningitis)
Some complications of Behçet’s are serious. Untreated eye inflammation can lead to decreased vision or even blindness. People with eye symptoms should have a full eye exam by an eye doctor (ophthalmologist). Blood clots that form in the extremities can lead to serious complications, as can inflammation of the blood vessels in the lung. Although rare, pulmonary artery aneurysm—an abnormal bulge in the artery wall that can burst—is the leading cause of death among Behçet’s patients. Inflammation in the membranes of the brain and spinal cord can lead to significant disability if untreated.
There is no single test for diagnosing Behçet’s syndrome. Your doctor will consider a number of factors including a detailed medical history, a physical exam, laboratory tests, imaging studies, and possibly a skin biopsy. The presence of classic Behçet’s symptoms, including recurrent mouth and genital sores, eye inflammation, and skin lesions, help confirm the diagnosis. The genetic marker HLA-B51 is more common among people with Behçet’s, but the presence of the gene alone is not diagnostic.
Laboratory or imaging tests may be ordered to rule out diseases with similar symptoms such as other forms of vasculitis (granulomatosis with polyangiitis and polyarteritis nodosa), inflammatory bowel disease, systemic lupus erythematosus, rheumatoid arthritis, Lyme disease and others.
Your doctor may also order a pathergy test, a procedure in which a small, sterile needle is inserted into the skin of the forearm. After 24 to 48 hours, people with Behçet’s can develop a lump or nodule at the needle insertion point, which indicates the immune system is overreacting to a minor injury. However, even a positive pathergy test is not conclusive.
Treatment for Behçet’s is aimed at reducing inflammation and preventing organ damage. Treatment depends on disease severity, symptoms, and organ involvement. The first line of treatment may include topical glucocorticoids applied directly to the affected area such as skin creams, gels and ointments, eye drops and mouth rinses. Oral glucocorticoids such as prednisone may also be prescribed to reduce inflammation. If topical or oral steroids aren’t effective, your doctor may prescribe other medications to fight inflammation including colchicine, which is commonly used to treat gout.
More severe disease may require immunosuppressive drugs such as methotrexate, azathioprine, cyclosporine, apremilast, and cyclophosphamide.
Biologics are also an option when Behçet’s is severe. Biologic medications are complex proteins derived from living organisms. They target certain parts of the immune system to control inflammation. Examples used to treat Behçet’s include infliximab, etanercept, adalimumab, and interferon alpha.
The medications used to treat Behçet’s have potentially serious side effects, such as lowering the body’s ability to fight infection, among others, so it is important to monitor your child’s symptoms and report them to the doctor. Infection prevention is also very important. Talk to the doctor about age-appropriate vaccinations, which can reduce your child’s risk of infection.
Even with effective treatment and periods of remission, some individuals will experience relapse of Behçet’s—sometimes months or even years after the original symptoms subside. If your initial symptoms return or you develop new ones, report them to your doctor as soon as possible. Regular doctor visits and ongoing monitoring of laboratory and imaging tests are important in detecting relapses early.
Effective treatment for Behçet’s may require the coordinated efforts and ongoing care of a team of providers and specialists. In addition to a primary care provider, Behçet’s patients may need to see the following specialists:
- Rheumatologist (joints, muscles, and immune system)
- Gynecologist (female reproductive system)
- Urologist (male reproductive system and urinary system)
- Dermatologist (skin)
- Ophthalmologist (eyes)
- Neurologist (brain and nervous system)
- Pulmonologist (lungs)
- Gastroenterologist (digestive system) or others as needed
The best way to manage your disease is to actively partner with your health care providers. Get to know the members of your health care team. It may be helpful to keep a health care journal to track medications, symptoms, test results and notes from doctor appointments in one place. To get the most out of your doctor visits, make a list of questions beforehand and bring along a supportive friend or family member to provide a second set of ears and take notes.
Remember, it’s up to you to be your own advocate. If you have concerns about your treatment plan, speak up. Your doctor may be able to adjust your dosage or offer different treatment options. It is always your right to seek a second opinion.
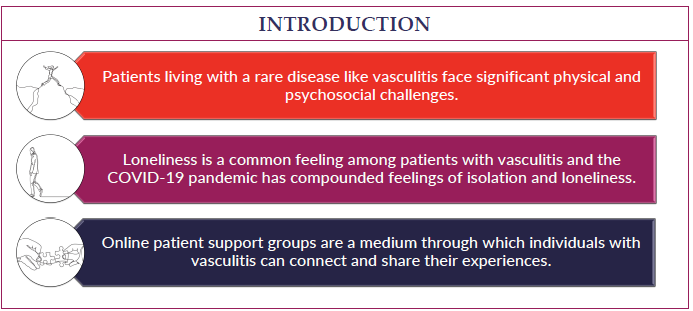
Living with Behçet’s can be challenging at times. Fatigue, pain, emotional stress, and medication side effects can take a toll on your sense of well-being, affecting relationships, work, and other aspects of your daily life. Sharing your experience with family and friends, connecting with others through a support group, or talking with a mental health professional can help.
There is no cure for Behçet’s syndrome at this time, but treatment can relieve symptoms and prevent potentially serious complications such as blindness and stroke. Behçet’s can be a chronic disorder with periods of remission and relapse, so most patients need to see a doctor on an ongoing basis.
American Behçet’s Disease Association: https://www.behcets.com/
John Hopkins Vasculitis Center: https://www.hopkinsvasculitis.org/types-vasculitis/behcets-disease/
Behçet’s Syndrome Videos
Patient Perspective: Living with Behcet's Disease