Vasculitis Types
About Rheumatoid Vasculitis
Last Updated on February 5, 2024
Rheumatoid vasculitis is a rare but serious complication of rheumatoid arthritis (RA)—an inflammatory disease that causes severe joint pain and damage, and can move beyond the joints to other parts of the body. When RA affects the blood vessels, it is called rheumatoid vasculitis. Vasculitis is a family of rare disorders characterized by inflammation of the blood vessels, which can restrict blood flow and damage vital organs and tissues. Rheumatoid vasculitis causes inflammation and narrowing of the small- and medium-sized blood vessels and most commonly affects the skin and nerves. However, it can involve virtually any organ in the body. People with RA who smoke may have a higher risk of developing this complication.

Quick Facts

4 cases per million worldwide

Number of US cases unknown

More common in older adults

Not seen in children

More common in males

Ethnic prevalence unknown
Rheumatoid vasculitis is a rare but serious complication of rheumatoid arthritis (RA)—an inflammatory disease that causes severe joint pain and damage, and can move beyond the joints to other parts of the body. When RA affects the blood vessels, it is called rheumatoid vasculitis. Vasculitis is a family of rare disorders characterized by inflammation of the blood vessels, which can restrict blood flow and damage vital organs and tissues. Rheumatoid vasculitis causes inflammation and narrowing of the small- and medium-sized blood vessels and most commonly affects the skin and nerves. However, it can involve virtually any organ in the body. People with RA who smoke may have a higher risk of developing this complication.
The primary symptoms of rheumatoid vasculitis include skin rash, small pits on the fingertips, or sores and redness around the nail, and numbness, tingling and pain of the hands and feet. Because rheumatoid vasculitis is systemic (affecting the whole body), it can also affect the heart, kidneys, gastrointestinal tract (GI), brain or lungs. Rheumatoid vasculitis resembles other forms of vasculitis including polyarteritis nodosa and cryoglobulinemic vasculitis.
With early diagnosis and treatment, it is possible to control symptoms of rheumatoid vasculitis and prevent or minimize organ damage. Treatment depends on disease severity and involvement of other organs. Mild disease affecting the skin is typically treated with glucocorticoids such as prednisone and/or other medications that suppress the immune system. More serious organ involvement may require higher doses of glucocorticoids and other powerful agents that control inflammation. Treatment decisions should consider the underlying RA. Drugs taken for RA may improve both the arthritis and vasculitis symptoms. Good control of the arthritis decreases the risk of rheumatoid vasculitis.
Rheumatoid vasculitis and RA are chronic diseases and even with treatment, relapses can occur, so ongoing medical care is necessary.
The cause of rheumatoid vasculitis, like other forms of vasculitis, is not fully understood. Vasculitis is classified as an autoimmune disorder—a disease that occurs when the body’s natural defense system mistakenly attacks healthy tissue. Researchers believe a combination of factors may set the inflammatory process in motion, including genetics, drug reactions, or an infection.
While the cause of rheumatoid vasculitis is yet unknown, several factors point to the likelihood of a person with RA developing it:
- Long-standing, severe RA, for 10 or more years
- High concentrations of “rheumatoid factor” antibodies, and the levels of certain other proteins in the blood
- Felty’s syndrome, a complication of RA characterized by an enlarged spleen and an abnormally low white cell count
- The presence of rheumatoid nodules, firm lumps under the skin around the joints of RA patients
- Smoking cigarettes, which may damage the lining of the blood vessels and predispose people to developing rheumatoid vasculitis
Rheumatoid vasculitis is rare, occurring in less than 1 percent of those who have RA, while RA is considered common and affects millions of people annually. It is estimated that 400 people per million develop RA per year, compared to less than 4 people per million who develop rheumatoid vasculitis.
Rheumatoid vasculitis appears to be more common in men than women, and typically affects individuals who have had severe RA for a decade or more. Rheumatoid vasculitis has been on the decrease for the past four decades with the advent of new effective treatment options for RA. Rheumatoid vasculitis can affect people from any ethnic background. Research has shown smokers are more likely to develop this form of vasculitis.
Symptoms of rheumatoid vasculitis depend on the parts of the body that are affected. Although it most commonly affects the skin and peripheral nerves, it can affect any organ and cause many different symptoms.
General symptoms of rheumatoid vasculitis include fever, fatigue, loss of appetite and weight loss, which are common symptoms of RA as well. Other symptoms include:
- Small pits in the fingertips, sores/ulcers around the fingernails
- A painful red rash, especially on the legs, or purplish bruises
- Tissue death (necrosis) of the fingers and toes if blood flow becomes totally blocked
- Numbness, tingling and pain, especially in the fingers and toes
- Muscle weakness
- Chest pain
- Abdominal pain
Although it is uncommon, serious, even life-threatening complications can occur if rheumatoid vasculitis affects major organs such as the heart, kidneys, lungs, GI tract or brain. These include:
- Heart attack
- Stroke
- Kidney failure
- Restriction of blood supply to the bowels
- Accelerated atherosclerosis
There is no single test to diagnose rheumatoid vasculitis. Your doctor will consider several factors including a detailed medical history, physical examination, laboratory tests (blood/urine), and specialized imaging studies. A tissue biopsy is typically required to make a definitive diagnosis.
Your doctor may suspect rheumatoid vasculitis based on the characteristic symptoms of rash, numbness and tingling of the extremities, skin ulcers, chest pain or other symptoms. Diagnosis also involves ruling out diseases that cause similar symptoms including other forms of vasculitis (polyarteritis nodosa and cryoglobulinemic vasculitis), diabetes, and atherosclerosis, which can also cause narrowing of blood vessels.
Depending on organs affected, the following diagnostic tests, or others, may be ordered:
- Blood tests: To detect abnormal levels of antibodies and proteins in the blood, which can indicate inflammation. People with rheumatoid vasculitis typically have elevated levels of rheumatoid factor antibodies, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR, or “sed rate”).
- Imaging tests: Chest X-ray, computed tomography (CT) or magnetic resonance imaging (MRI) scans of brain, chest or abdomen, angiogram (X-ray of blood vessel after injection of contrast dye).
- Electrocardiogram (ECG): To check heart rhythm.
- Endoscopy: An examination of the esophagus, stomach, and portions of the intestine with a lighted, flexible instrument called an endoscope.
- Electroneuromyography (EMG): To test nerve function.
- Tissue biopsy (usually required to confirm the diagnosis): This surgical procedure removes a small tissue sample from an affected vessel (skin ulcer, nerve or muscle), which is examined under a microscope for signs of inflammation or tissue damage.
The course of treatment for rheumatoid vasculitis depends on the severity of vasculitis and organs involved. Any treatment decisions should consider the underlying RA and how it is being treated. Drugs taken for RA may improve both joint symptoms and the vasculitis.
For mild symptoms of rheumatoid vasculitis such as fingertip sores, treatment involves protecting the area to prevent infection and use of glucocorticoids such as prednisone. For more widespread disease, glucocorticoids may be used in combination with other immunosuppressive medications such as methotrexate or azathioprine. More serious organ involvement may require higher doses of glucocorticoids, cyclophosphamide (a chemotherapy-type drug), or biologic agents such as rituximab, abatacept, or others. Biologic medications are complex proteins derived from living organisms and target certain parts of the immune system to control inflammation.
Research has shown that rheumatoid vasculitis is associated with smoking. If you have RA and are a smoker, stopping smoking may reduce the risk of developing rheumatoid vasculitis.
The medications used to treat rheumatoid vasculitis and RA have potentially serious side effects such as lowering the body’s ability to fight infection, and potential bone loss (osteoporosis), among others. Therefore, it’s important to see your doctor for regular checkups. Medications may be prescribed to offset side effects. Infection prevention is also very important. Talk to your doctor about getting vaccines (e.g., flu shot, pneumonia and/or shingles vaccination), which can reduce your risk of infection.
Even with effective treatment, relapses can occur with rheumatoid vasculitis. If your symptoms return or you develop new ones, report them to your doctor as soon as possible. Regular doctor visits and ongoing monitoring of lab and imaging tests are important in detecting relapses early.
Effective treatment of rheumatoid vasculitis may require the coordinated efforts and ongoing care of a team of medical providers and specialists. In addition to a primary care provider, you may need to see the following specialists:
- Rheumatologist (joints, muscles, immune system)
- Dermatologist (skin)
- Neurologist (nerves)
- Ophthalmologist (eyes)
- Gastroenterologist (digestive system)
- Cardiologist (heart)
- Pulmonologist (lungs) or others as needed
The best way to manage your disease is to actively partner with your health care providers. Get to know the members of the health care team. It may be helpful to keep a health care journal to track your medications, symptoms, test results and notes from doctor appointments in one place. To get the most out of your doctor visits, make a list of questions beforehand and bring along a supportive friend or family member if necessary to provide a second set of ears and take notes.
Remember, it’s up to you to be your own advocate. If you have concerns about your treatment plan, be sure to speak with your medical team. Your doctor may be able to adjust your dosage or offer different treatment options. It is always your right to seek a second opinion.
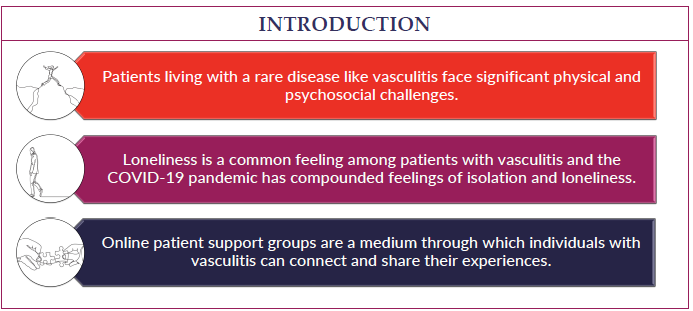
Living with a serious health condition such as rheumatoid vasculitis can be overwhelming at times. Fatigue, pain, emotional stress, and medication side effects can take a toll on your sense of well-being, affecting relationships, work, and other aspects of your daily life. Sharing your experience with family and friends, connecting with others through a support group, or talking with a mental health professional can help.
Rheumatoid vasculitis is one of the most serious complications of long-standing RA, and prognosis depends on disease severity and organ involvement. Some patients have milder symptoms while others can develop serious complications including heart failure, kidney failure and stroke, among others. Early diagnosis and treatment are essential in controlling the disease and preventing damage to blood vessels, vital tissues, and organs. Not smoking may reduce the risk of developing rheumatoid vasculitis.
The incidence of rheumatoid vasculitis has decreased over the past 40 years due to improved RA treatments including widespread use of biologic therapies.