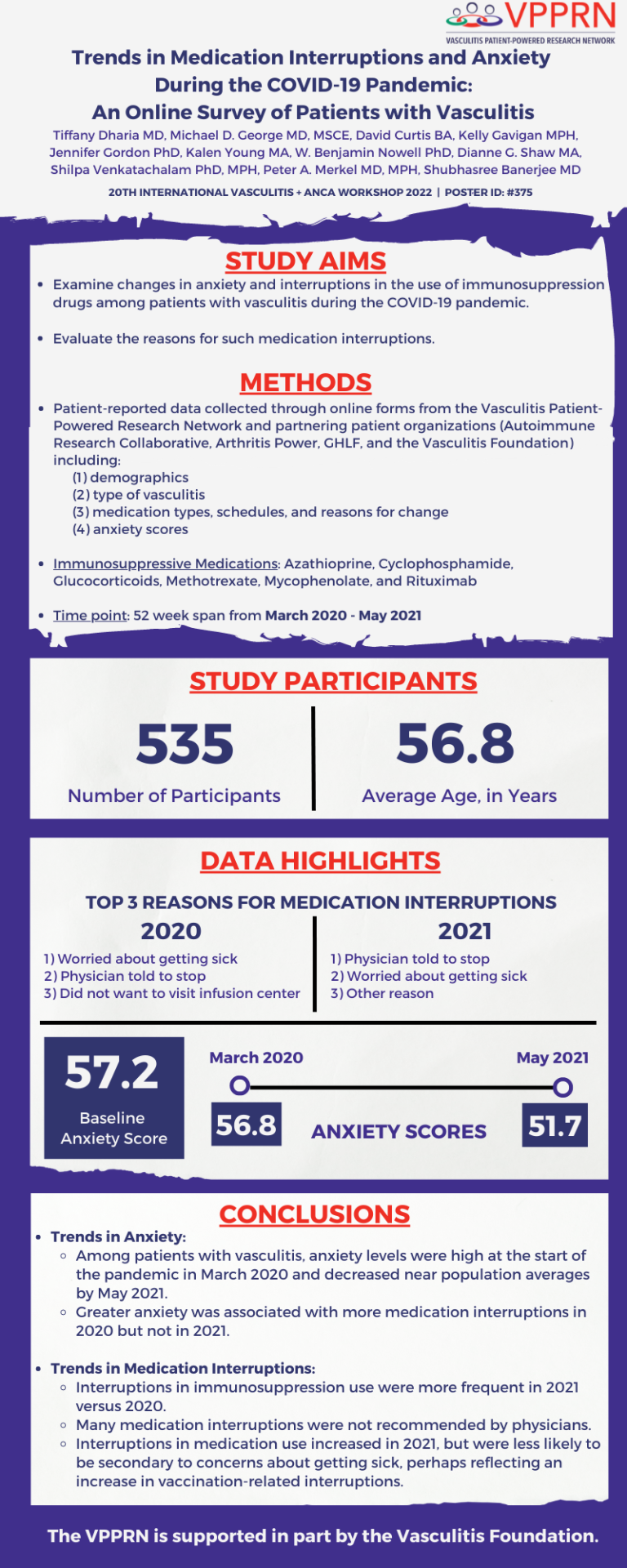
Research Abstract

Vasculitis Patient-Powered Research Network (VPPRN) Research Abstract
Vasculitis and ANCA Workshop | April 2022 | Dublin, Ireland
As part of the 20th International Vasculitis and ANCA Workshop, our investigators examined changes in anxiety and interruptions in the use of immunosuppression medications among patients with vasculitis during the COVID-19 pandemic, along with the reasons for such medication interruptions.
Take a look at what our investigators found out!
Also, take a few minutes to get to know are investigators as well – their bios are available below.

VPPRN Research Abstract
Get to Know Our VPPRN Investigators

Tiffany Dharia, MD
Tell us about yourself, your research and why this interests you.
I am a third year Internal Medicine resident at the Hospital of the University of Pennsylvania. My interests lie in immunology, systemic autoimmune disease and health equity. My research is of particular interest because COVID-19 has been a significant source of anxiety for many of our patients. It was important for us to see how their behavior changed over the course of the pandemic and how this was reflected in health outcomes. I am interested in identifying barriers to patient care and furthering understanding of patient behaviors and outcomes.
Fun fact: I have visited all the 7 wonders of the world!
Michael George, MD, MSCE
Tell us about yourself, your research and why this interests you.
I am an Assistant Professor in Rheumatology and Epidemiology at the University of Pennsylvania. My research is focused on better understanding the safety of glucocorticoids and other immunosuppression with a particular interest in infections. The VPPRN project has been a great chance to explore how patient concerns about a specific infection, COVID-19, has affected their medication use and health.
Fun fact: My college ultimate frisbee team competed in college nationals.
Who Made this Research Possible?
YOU DID!
It is because of the continued participation and engagement of our VPPRN members that research studies like this are possible.
YOUR Data = NEW Research + NEW Treatments
The more people participate, the more data is available to help clinicians and researchers better understand vasculitis.
Your data drives research & we cannot do our research without you!
Not a VPPRN member? Let’s change that! Simply select the Join the Registry button to be taken to our online consent form. We’re excited to have you join the VPPRN community!
Already a VPPRN Member? Click the Login button below to login to your account.